Written by Dr Marcus Ng (Osteopath) M. Osteo, B App Sc (Osteo Studies), B. Sc (Anat.)
Let’s start by discussing what osteopathy is and the underlying principles it is governed by.
What is Osteopathy?
Osteopathy is a manual (hands-on) treatment of the body to improve its capacity to function. Osteopaths use a variety of techniques to treat which can be classified as “Active” and “Passive”.
Active techniques are where the patient primarily does an intervention, such as exercise rehabilitation. Ppassive techniques are where the osteopath performs the intervention, while the patient is less actively involved.. These techniques include soft tissue massage, joint mobilisation and manipulation.
What are the principles of Osteopathy?
The four principles of osteopathy are:
- The body is a unit.
- The mind, body, and spirit are interconnected.
- Physical health is influenced by mental and emotional well-being, and vice versa.
- Osteopaths consider all aspects of a person, not just the site of pain, when diagnosing and treating.
- Structure and function are interrelated.
- How the body is built (structure) affects how it works (function), and vice versa. For example, restricted joint movement or poor posture can impair circulation, nerve function, and overall mobility.
- Osteopaths look for restrictions or imbalances in the body that may be affecting health or performance.
- The body has the capacity to self-regulate and has self-healing mechanisms.
- The body has an innate ability to maintain health and recover from illness or injury.
- Osteopathic treatment aims to support and enhance these natural processes rather than override them.
- Treatment should be based on the above three principles.
- Osteopaths use their knowledge of anatomy, physiology, pathology, and biomechanics to create individualised treatment plans.
- The goal is not just symptom relief, but to restore function, support overall health, and empower the patient.
What is Evidence-Based Practice (EBP)?
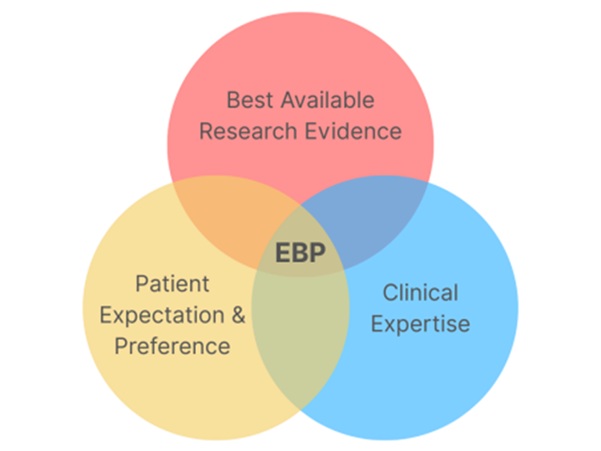
Evidence-based practice (EBP) is a systematic approach to decision-making that utilises the best available evidence, including research findings, clinical expertise, and patient values, to guide practice.
It involves integrating the following elements to make informed decisions that can lead to improved outcomes.
- Best available research evidence: This refers to clinically relevant research from studies with minimal bias, like randomised controlled trials.
- Clinical expertise: This encompasses the knowledge, skills, and experience of the healthcare professional.
- Patient expectations and preferences: Acknowledging and incorporating the patient’s preferences and circumstances into the decision-making process.
Relation between Osteopathy and EBP
With the terms defined, here is what we know of osteopathy as an evidence-based approach in treating patients. When treating musculoskeletal dysfunctions like back pain and neck pain, osteopathy does have research-backed evidence to support it.
Back Pain
According to research published in BMJ Open and The Lancet, manual therapy, including spinal manipulation and mobilisation, can be an effective part of a multi-modal approach for managing back pain.
A 2020 systematic review showed that osteopathic manipulative treatment significantly improved pain and disability in patients with chronic low back pain. When combined with exercise and education, these treatments are especially beneficial.
Neck Pain
Neck pain, often caused by poor posture, stress, or prolonged sitting, responds well to manual techniques like joint mobilisation, soft tissue massage, and muscle energy techniques, all commonly used in osteopathy. Studies indicate short-term improvements in pain and range of motion, especially when patients stay active and involved in their treatment.
It should be noted that in some of the research conducted on the benefits of different manual therapy techniques, both active and passive techniques are not categorised specifically as ‘osteopathy’ only, ‘chiropractic’ only or ‘physiotherapy’ only techniques. This means that, with the appropriate training and expertise, any practitioner can perform these techniques within their scope of qualifications.. This may often raise the common question: I have an injury, who should I see – an osteopath or a physiotherapist? (insert separate Blog Link )
While there is evidence supporting osteopathic treatment for back and neck pain—particularly through active and passive manual techniques—let’s shift focus to other conditions where research may be limited, but clinical expertise and anecdotal evidence suggest patients can still benefit.
Headaches and Migraine
Headaches and migraine are common presentations in the clinic. Some tension-type and cervicogenic headaches are linked to musculoskeletal dysfunction in the neck and upper back. Osteopaths may use gentle manual therapy to release tension in these areas, which can reduce headache frequency and intensity. Migraine management through osteopathy still lacks strong research evidence and should be approached cautiously, but this is where an experienced osteopath can use their expertise to help, using a variety of techniques.
Pregnancy
Pregnancy-related pain often comes with musculoskeletal discomfort. Think ligament laxity through shifting hormonal changes, pelvic girdle pain, sciatica, and lower back tension. Osteopathic treatment during pregnancy has been shown in small studies to improve functional outcomes and reduce pain, potentially making pregnancy more comfortable without medication. Anecdotally, patients may find these symptoms worsen during the second and third trimesters, and passive techniques during this time have been very helpful in easing discomfort.
Patient Preferences is the last pillar of EBP model. This is something an osteopath can find out before the commencement of any treatment. A written and verbal consent should be given and the osteopath must adhere to such requests. For example, suppose a patient has had some ill effects from a manipulation from previous treatments or has fears after hearing from friends or family who suffered poor outcomes after said technique. In that case, the osteopath must take this into consideration to weigh up the risk versus reward of performing such a technique. This is why an osteopath with extended clinical experience and expertise in various techniques is so important.
Cranial and Visceral Osteopathy
A word on a less common and perhaps “old school” branch of osteopathy — both cranial and visceral osteopathy have much less scientific backing. While some practitioners and patients swear by their effectiveness, large-scale and high-quality clinical trials haven’t consistently shown strong evidence for these methods.
Cranial osteopathy, also known as craniosacral therapy, is a specialised area of osteopathy that focuses on the delicate movements and structures of the skull and its surrounding tissues. Osteopaths practising cranial osteopathy use a highly developed sense of touch to identify and address restrictions or imbalances in the cranial bones, meninges, and cerebrospinal fluid. This approach aims to enhance the body’s self-healing mechanisms and improve overall well-being.
Visceral osteopathy is a manual therapy technique within osteopathy that focuses on the internal organs (viscera) and their relationship with the musculoskeletal system. It involves gentle manipulations to improve organ mobility, release tension in fascial tissues, and address potential restrictions that may contribute to musculoskeletal or digestive issues.
Conclusion
Is osteopathy evidence-based? In short, it depends… While manual (active and passive) techniques such as joint mobilisation, soft tissue massage, and spinal manipulation along with exercise prescription and education, have shown to be beneficial, there is currently less evidence to support Cranial and Visceral branches of osteopathy.
Ultimately, any form of treatment for best patient outcomes must be through the three pillars of Evidence-Based Practice; the intersection of best available research evidence, clinical expertise of the treating osteopath, while considering patient expectations and preferences.
If you’re curious about how osteopathy could help you, book an appointment at Quay Health in Sydney today—our experienced osteopaths will work with you to find a personalised treatment approach that’s informed, collaborative, and aligned with your goals.
References
Licciardone, J. C., Kearns, C. M., Minotti, D. E., & Tatman, L. H. (2020). Osteopathic manipulative treatment for chronic low back pain: A randomized controlled trial.
Journal of the American Osteopathic Association, 120(8), 529–538. https://doi.org/10.7556/jaoa.2020.088
Foster, N. E., Anema, J. R., Cherkin, D., Chou, R., Cohen, S. P., Gross, D. P., … & Maher, C. G. (2018).
Prevention and treatment of low back pain: evidence, challenges, and promising directions. The Lancet, 391(10137), 2368–2383. https://doi.org/10.1016/S0140-6736(18)30489-6
Franke, H., Franke, J. D., & Fryer, G. (2014).
Osteopathic manipulative treatment for nonspecific low back pain: A systematic review and meta-analysis.
BMC Musculoskeletal Disorders, 15, 286. https://doi.org/10.1186/1471-2474-15-286
Miller, J., Gross, A., D’Sylva, J., Burnie, S. J., Goldsmith, C. H., Graham, N., … & Kay, T. M. (2010).
Manual therapy and exercise for neck pain: A systematic review.
Manual Therapy, 15(4), 334–354. https://doi.org/10.1016/j.math.2010.03.008
Licciardone, J. C., Aryal, S., & Singh, K. P. (2010).
Osteopathic manipulative treatment for chronic low back pain: A randomized controlled trial.
The Journal of the American Osteopathic Association, 110(10), 646–656. Green, C., Martin, C. W., Bassett, K., & Kazanjian, A. (1999).
A systematic review of craniosacral therapy: Biological plausibility, assessment reliability and clinical effectiveness.
Complementary Therapies in Medicine, 7(4), 201–207. https://doi.org/10.1016/S0965- 2299(99)80003-9
Guillaud, A., Darbois, N., Monvoisin, R., & Pinsault, N. (2018).
Effectiveness of visceral osteopathy: A systematic review of the literature. European Journal of Osteopathic Research, 7, 1–10.




