What is Greater Trochanteric Pain Syndrome?
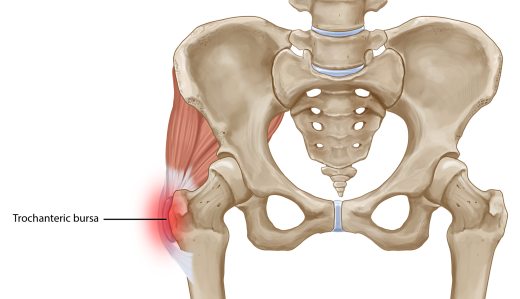
Pain on the outside of the hip is often referred to as Greater Trochanteric Pain Syndrome (GTPS) and was traditionally diagnosed as Trochanteric Bursitis, however, recent research defines non-inflammatory tendinopathy of the gluteus medius and/or gluteus minimus muscles to be the main source of lateral hip pain. Therefore GTPS is more of a degenerative condition rather than inflammatory.
GTPS is a syndrome defined by tenderness to palpation over the greater trochanter with the patient in the side-lying position. This condition affects both athletes (particularly runners) and less active people. One out of four females over 50 years is likely to be affected.
Symptoms of Greater Trochanteric Pain Syndrome?
Pain on palpation of the outside of the hip is a main diagnostic indicator of greater trochanteric pain syndrome. Usually it will come on slowly, gradually worsens with time and with different loads and tasks. It gets worse at night and sleeping on the affected side worsens the symptoms, affecting the quality of sleep.
GTPS has significant impacts on the quality of life, with similar symptoms to those of hip Osteoarthritis. It interferes with sleep (side lying) and common weight bearing tasks.
Patients usually report pain with single-loading tasks such as walking and going up/ down stairs. Tasks that require active hip extension, such as sit to stand, are also accompanied with pain and stiffnes of Greater Trochanteric Pain Syndrome?
How is Greater Trochanteric Pain Syndrome diagnosed?
Greater Trochanteric Pain Syndrome is diagnosed by an Osteopath, Chiropractor or Physiotherapist. Your practitioner can diagnose you by doing a functional assessment, looking at the biomechanics of the lower limb, as well as some orthopaedic testing locally to the hip. Being able to reproduce pain on the outside of the hip, by either palpating the area, or by activating the muscles is a positive diagnosis.

How is Greater Trochanteric Pain Syndrome treated?
Your Osteopath, Chiropractor or Physiotherapist, will be able to diagnose your hip pain and will provide a treatment plan for your condition. This may involve hands on techniques: massage, stretching and joint manipulation and may include the following treatments:
Ice and heat:
Ice and heat can help to alleviate the pain, as can sleeping with a pillow between the legs, however loading the tendon will give long lasting results.
Strengthening and Functional exercises:
Combined strengthening and functional exercises to optimise movement control patterns and obtain pelvic control have been proven to give the most effective results.
Isometric exercises can give a pain-relieving effect, but inhibiting pain pathways, therefore they are used for pain management. Low load, low velocity isometric hip abduction may be performed side-lying, supine and standing positions for multidirectional training. For example, Glute bridges, or single leg squats.
Corticosteroid injections:
Corticosteroid injections provide a short term pain relieving effect although the pain doesn’t resolve completely and and often recurs. Corticosteroids exhibit non-inflammatory effects and GTPS is reported to be a degenerative condition rather than inflammatory. The pain relieving effect following corticosteroids might interfere with the tendon capacity to respond appropriately to loading.
Surgery:
90% of patients who had a gluteal tendon repair surgery reported long lasting pain relief. Furthermore, removal of trochanteric bursae and ITB release is utilised in patients without gluteal tears. Studies have been shown to report good to excellent short-medium term outcomes.




